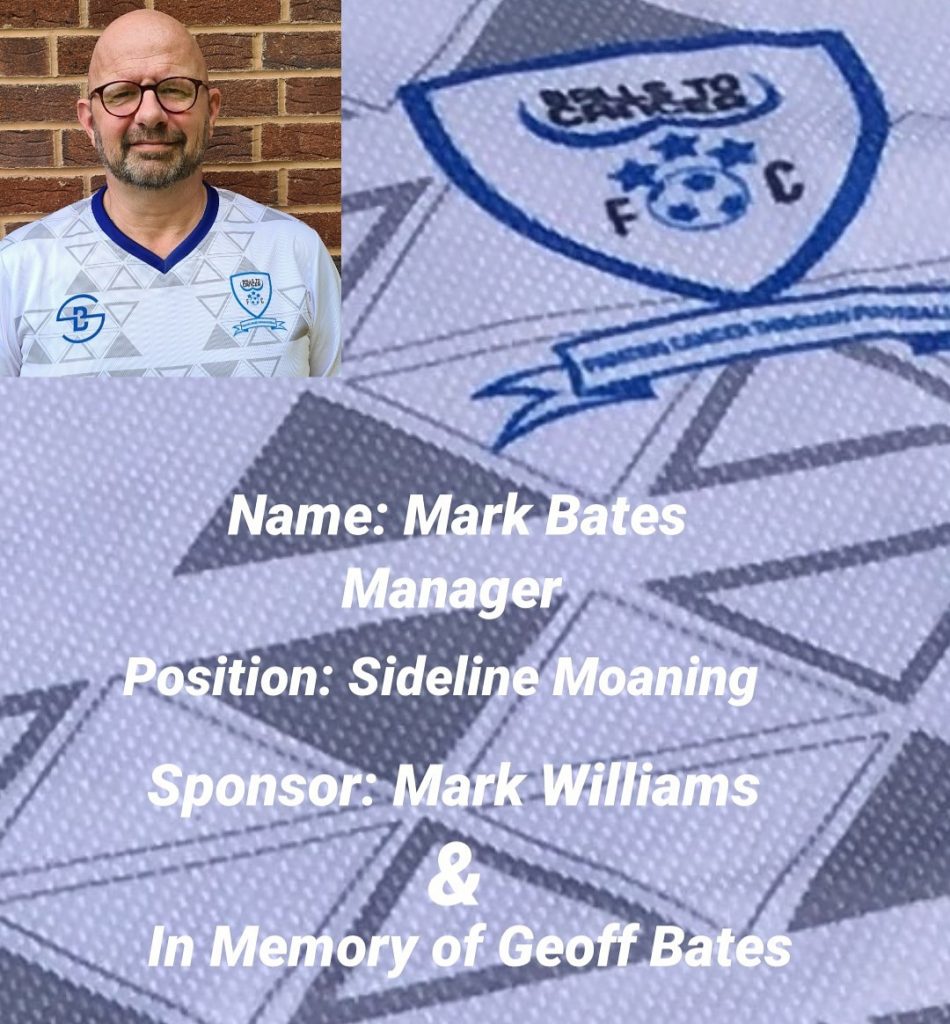
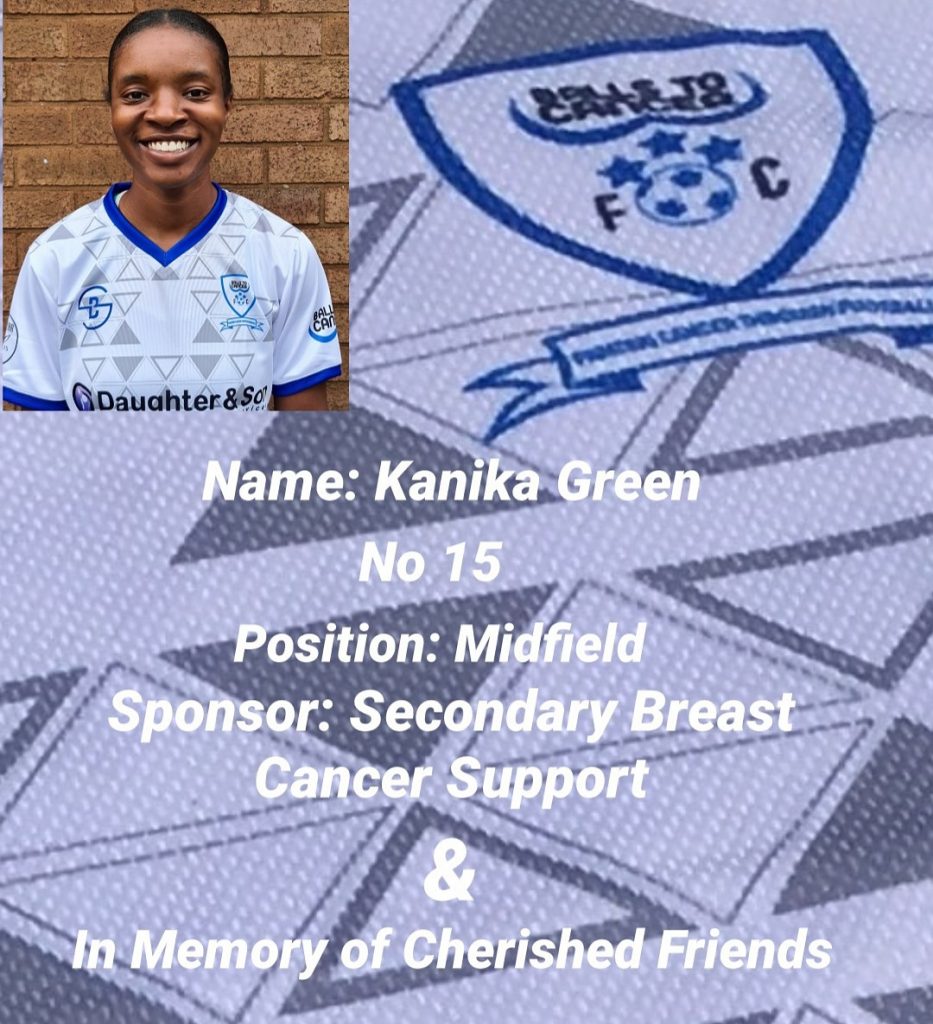
Please meet the BTC Ladies for season 20/21.
The Ladies team are sponsored by Daughter And Son Washing Services, Davies Domestic Appliances and X21 Clothing





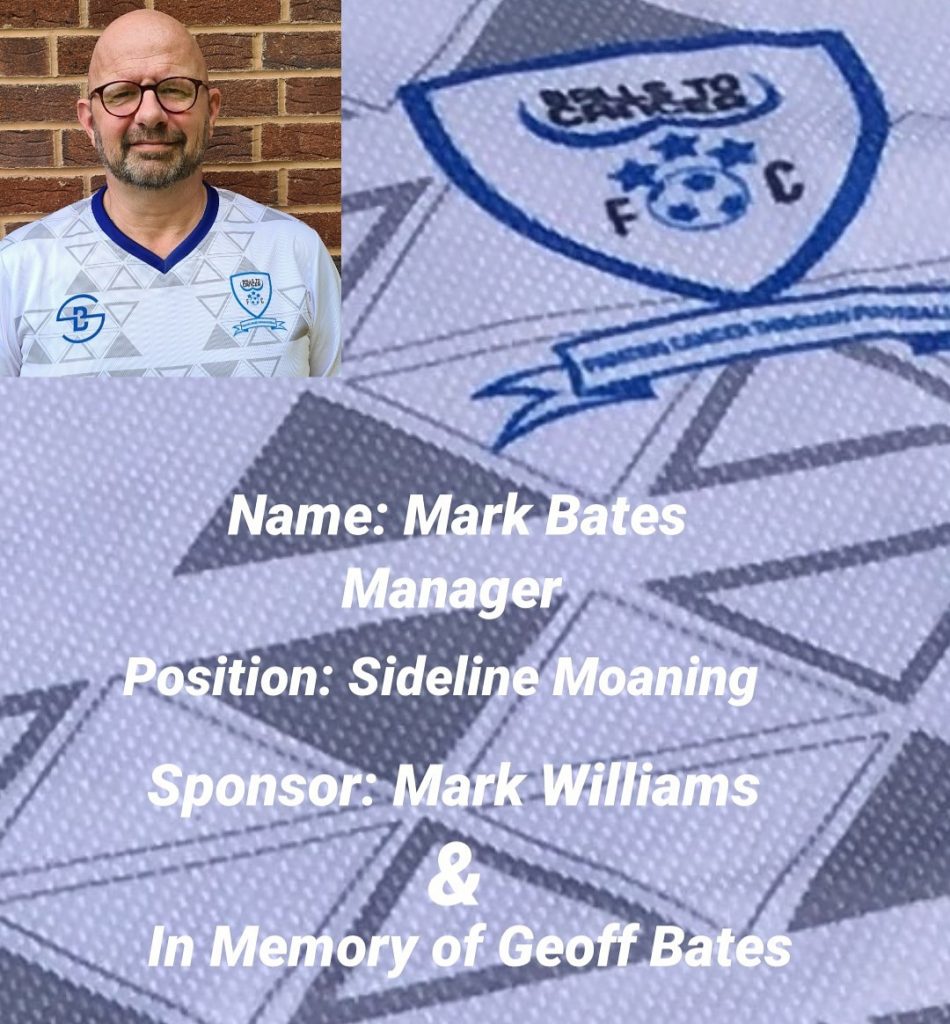


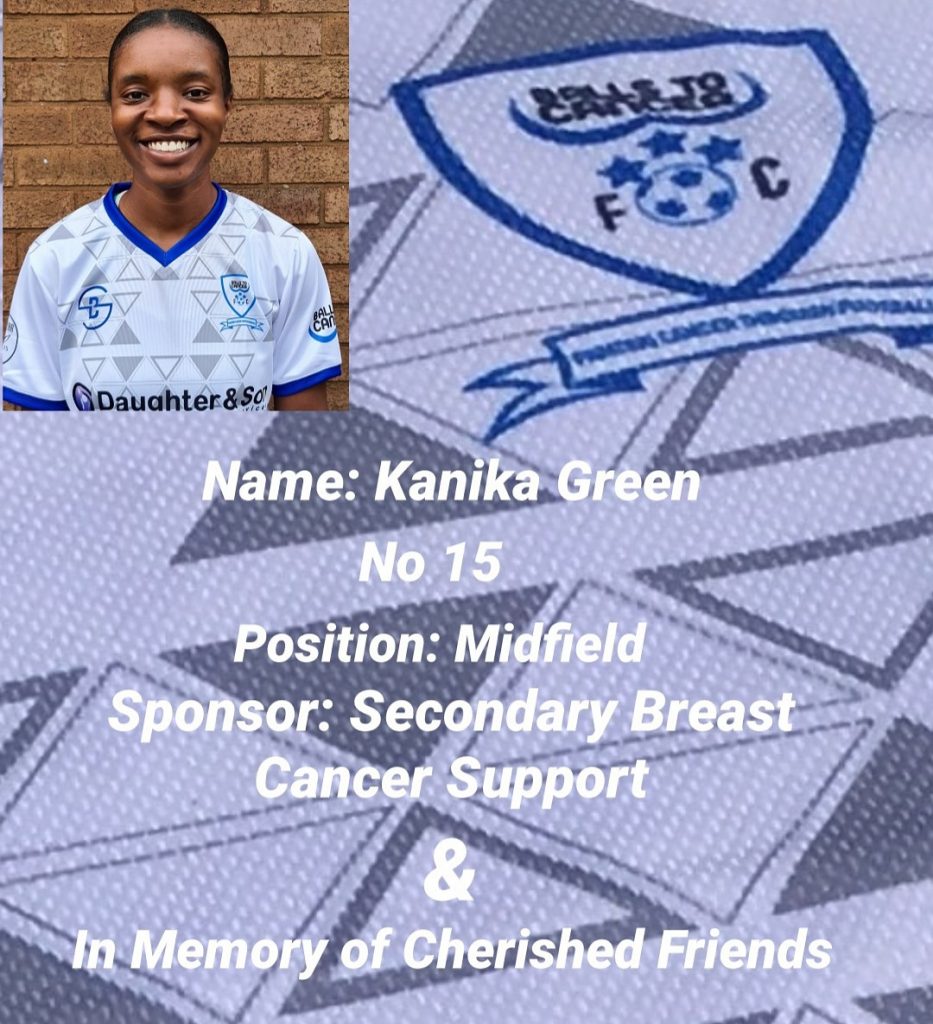



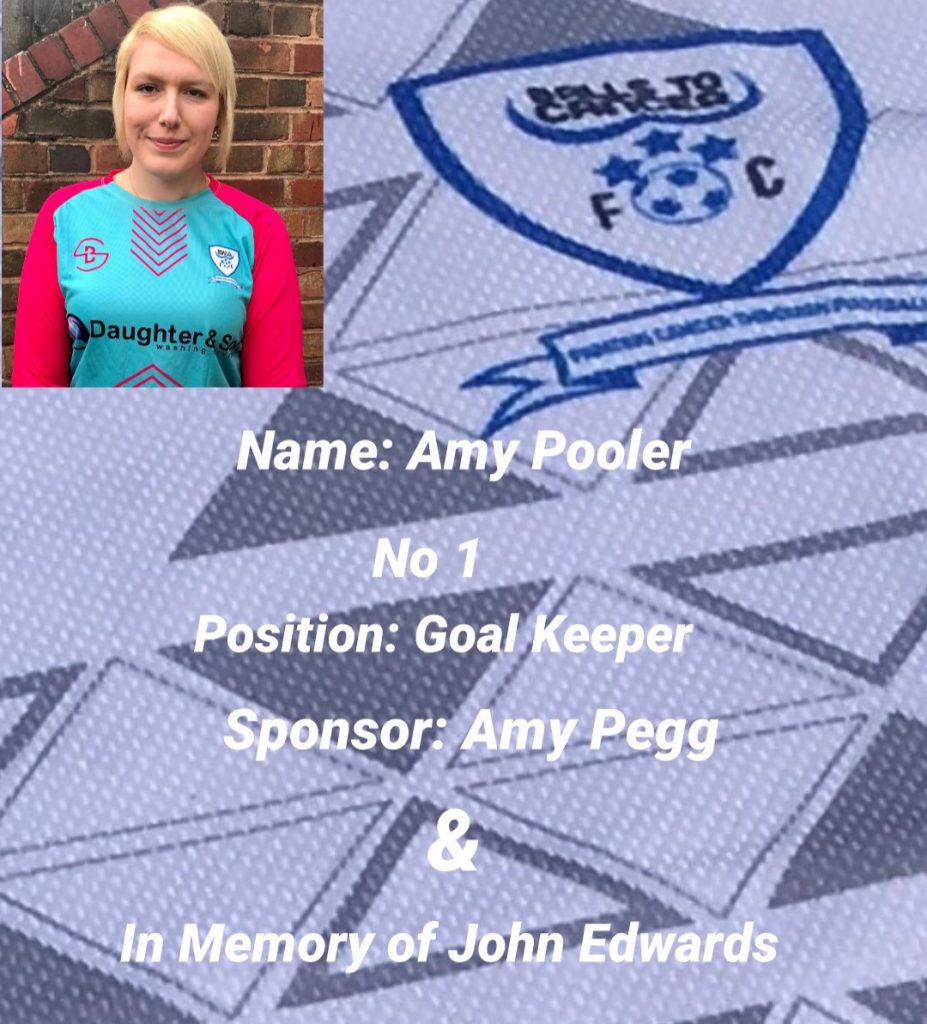


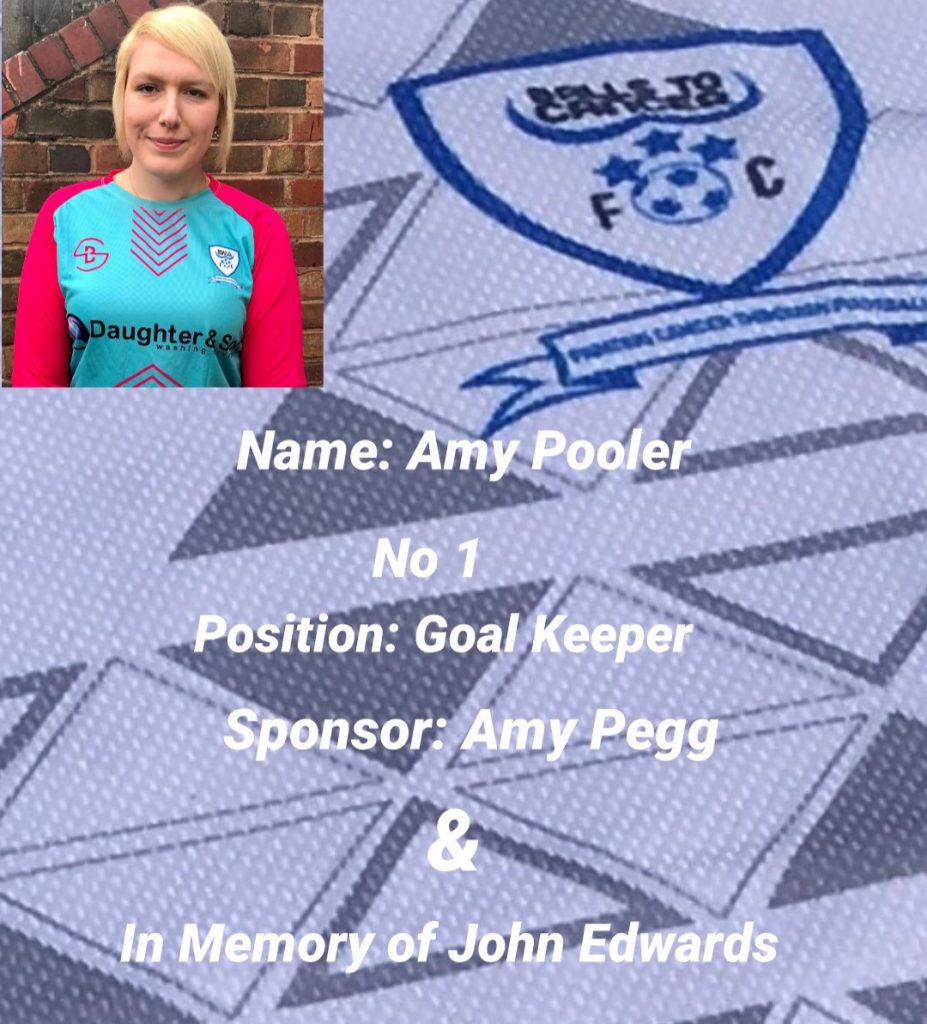
Please meet the BTC Ladies for season 20/21.
The Ladies team are sponsored by Daughter And Son Washing Services, Davies Domestic Appliances and X21 Clothing












Prostate cancer is the most common cancer in men in the UK. Although it affects all men, black men are 2-3 times more likely to develop this cancer than their white counterparts. The death rate is twice as high. Furthermore, black men are more likely to develop prostate cancer at a younger age.
It is essential that black men, in particular, know about their increased risk of prostate cancer.
Why it is more common is unknown; there is much research worldwide to discover the reason.
Every black man over the age of 45 years is eligible to have the blood test, called PSA (prostate specific antigen) from their GP. All he need do is to request one from the GP and have a discussion about it. Every GP in the land has been sent a document called the Prostate Cancer Risk Management Programme, which says that men, even with no urinary symptoms, can have a PSA on request. There are some limitations of the blood test which the GP can point out. For example, a raised PSA (above 3 units) does not necessarily mean that there is prostate cancer. There are other reasons why a PSA may be raised.
More often than not, prostate cancer in its early and therefore curable stage does not present with symptoms, hence the importance of the blood test. Some men will have urinary symptoms, such as a slow urinary stream or passing urine frequently, or getting up at night, or having to get to the toilet in a hurry. These do not mean the man has prostate cancer. Far more common is an enlarged prostate gland that occurs as men age. However, as these symptoms are indistinguishable from those of prostate cancer, they should be checked out by a health care professional.
Black men face an increased risk of prostate cancer so a lack of urinary symptoms, should not be the basis for refusing to conduct a PSA test.
It is also worth noting that prostate cancer can run in families. So, if a first-degree relative, such as a father or brother, has prostate cancer, your risk is doubled. A family history of prostate cancer is therefore a reason for asking for a PSA blood test. A digital rectal examination is off-putting for many men. However, it can detect a problem with the prostate gland even where the PSA is normal. However, the PSA is more useful. Men should at least have the blood test even though they may decline the rectal examination (which is the only way of feeling the prostate).
A suspicion of prostate cancer, whether on account of an abnormal blood PSA or an abnormal feeling prostate on rectal examination, will lead to an urgent referral to see an urologist. Further tests include a MRI scan and a biopsy of the prostate gland. A biopsy is where samples of the prostate gland are taken and analysed in the laboratory for signs of cancer.
If cancer is diagnosed, keeping an eye on it may be advised as many prostate cancers will never cause a problem (‘active surveillance’). If there is more than a minimal amount of cancer a more aggressive treatment may be recommended, such as surgery or radiotherapy.
The success rate of treatment is very high when prostate cancer is detected early. Even if the disease has spread (called metastasized) there are good treatment options, if not necessarily curative.
In summary, black men are at increased risk of prostate cancer. I would urge all black men over 45 years old or even younger if someone in the family has had prostate cancer, to get themselves a PSA blood test from their GP. The cure rate is very high when the disease is found early. This Men’s Health Week I’m urging everyone to talk about prostate cancer, and prostate cancer in black men and their family background
My Story starts at the age of 17, I was a carefree teenager who never ever got ill, It was 2004 and the year before I had enjoyed a wonderful family holiday in Australia & was also settling into my first job.
Until June 2014 when my life flipped upside down, I noticed a lump in my shorts, At first I ignored it unaware of what it was, In those days I played a lot of sport and merely put it down to a sporting injury.
A few weeks past without a sign of it clearing up so I confided in my Mum who suggested I went to the doctor which in the end despite being embarrassed I reluctantly did.
My doctor was hopeful at first it looks like ‘You got water on your testicles’ He felt I had a condition called Hydrocele but sent me for a ultrasound scan in a nearby sports clinic.
The scan was done and I was instantly rushed back to the doctors, I felt that was a strange move but had no idea why. Once back at the doctors the news broke, ‘Aaron I’m sorry to have to tell you this you have Cancer’
I was stunned to silence unaware of what was happening, Nothing processed I had never been ill & now I was being told I had Cancer?
I was a very strong 17 year old and I battled my illness with positively. Yes I had a testicle removed at a young age but i took everything in my stride.
Cancer treatment followed in Mount Vernon hospital, My professor was a leader in the Testicular Cancer field Professor Rustin.
Words by Professor Karol Sikora, Consultant Oncologist and Medical Director, Rutherford Cancer Centres and former Director of WHO Cancer Programme
Some 30,000 people each month are normally found to have cancer and around 450 a day sadly die from the disease. There are no peaks or troughs – just a flat line which refuses to budge.
But over the last three months the number of people diagnosed has fallen precipitously. My estimate is that less than a third of the expected number of patients have been diagnosed.
Several studies – one from Cancer Research UK, one from Kings College and yet another from University College suggest a similar number. So where are the missing patients and why does it matter?
Rates of cancer in this country haven’t just dropped off a cliff, the disease will be growing, undetected, in thousands of people. They’re just not being diagnosed.
Frankly, I’m astounded more hasn’t been done. The whole reason I got involved in the coronavirus debate was to stand up for the forgotten cancer patients, everything I feared back then has happened, perhaps even worse than I imagined.
Cancer doesn’t care about pandemics – it has its own very different agenda, it’s the unseen enemy within.
The causes of cancer are multiple, but the result is the same – the subversion of the growth control processes of a cell. The rogue cells multiply and spread beyond the confines of the organ in which they arose. Breast, colon, prostate and lung are the four commonest sites, but all organs can be affected.
Spread of cancer by a process called metastasis (from Greek meaning change of place) is lethal. Cancer cells can grow outside the organ from which they arose spreading via the lymphatic system and blood to lungs, liver, brain and bone. They leave a trail of destruction which eventually kills.
We do have effective therapies – surgery, radiotherapy, chemotherapy and immune treatments but they all work best when the disease is localised.
Delay makes spread more likely and so the outcome of treatment will be significantly poorer. It also means that optimal care will be longer, more challenging and result in more side effects.
So here we are nearly four months into the pandemic and the numbers of new cancer patients are still frighteningly low.
The numbers of patients consulting with GPs are slowly climbing but not nearly quick enough, continued delays in the diagnostic pathway, difficulties in scheduling surgery. So tens of thousands of people aren’t being diagnosed, and many of those who do find they aren’t getting treatment as quickly as they should.
At the start of the pandemic I would always talk in hypothetical terms about cancer, sadly it’s no longer a possibility, it’s happening.
The delays are inevitably causing upward stage migration in many patients. I’ve had far too many difficult conversations about a patient’s prognosis with them, I expect to have many more over the coming months.
There are lots of concerns around a second wave of coronavirus, and the country is rightly preparing for that but my concern is a tsunami of cancer, cardiac and other patients with serious illnesses who have been neglected the last few months.
For cancer, I expect it will come around September. If we aren’t ready the dam will burst with catastrophic effects.
My concern is a tsunami of cancer, cardiac and other patients with serious illnesses who have been neglected the last few months. Professor Karol Sikora
The backlog of cancer cases due to Covid-19 will require an emergency national response similar to the response to Covid-19 itself to prevent a full-blown health crisis in the coming months.
The stage migration of cancer with poorer outcomes was somewhat inevitable but the figures are worse than I anticipated.
So how do we fix it? We need solutions.
We desperately need to find a balance between fear and caution. When people are too frightened to get a persistent symptom checked out for fear of catching the virus, we must have gone wrong somewhere. Of course everyone needs to be careful, but leaving a symptom unchecked could be a deadly mistake.
Back at the start of this pandemic I wrote for ITV Newstrying to sound the alarm. I wasn’t listened to and we are now seeing the consequences.
I’ve tried to steer away from apocalyptic predictions for good reason, but I will make my own now. Unless something drastically changes and quickly, in a few years we will look back in horror at the number of people we lost needlessly to cancer. People have suggested 35,000 fatalities, I suspect it could be far higher.
An spokesperson for the NHS said: “More than 350,000 people received an urgent hospital check and 65,000 people started treatment for cancer through the peak of the pandemic, and after an entirely appropriate and necessary pausing of some screening and treatments to protect patients from the risk of the virus, the NHS is taking urgent action to increase the number of tests and treatment carried out so that more people are able to be seen quickly and safely.
“The critical point remains that anyone with a possible symptom should come forward for a check-up with their GP as they normally would.”
Source: ITV.com
We are very pleased to announce the launch of our replica football shirts.
Not only do we have the home shirt but also the away, goalkeeper, hoodie, coat, tee shirts etc…. all supplied by the brilliant Sportybits.co.uk
Anything you purchase gets a donation made to BTC so not only are you supporting the team but also the charity.
Take a look at the range here









As we approach the beginning of the 20/21 grassroots football season we are very pleased to announce that we have a new team to add to our existing Adult mens and womens teams.
We have a brilliant new under 15s boys team managed by Dean Thomas. We look forward to seeing them grow and hopefully have a great first season.
We are committed to adding more boys and girls team as soon as we can. If you know of a team or players looking for a new home then please contact us ASAP.
Today we have agreed to join the fantastic One Lottery system.
So from today you can buy tickets at just £1 each to be entered into our August draw where you could win £25,000!!!
So as they say ” You have to be in it to win it ” get your tickets here

With the help of our brilliant kit suppliers Sporty Bits, we have been able to produce an amazing Balls to Cancer football kit available in various colours.
We have produced this kit in answer to calls from our supporters for a kit they can wear to support the charity.
The kits are available to buy here

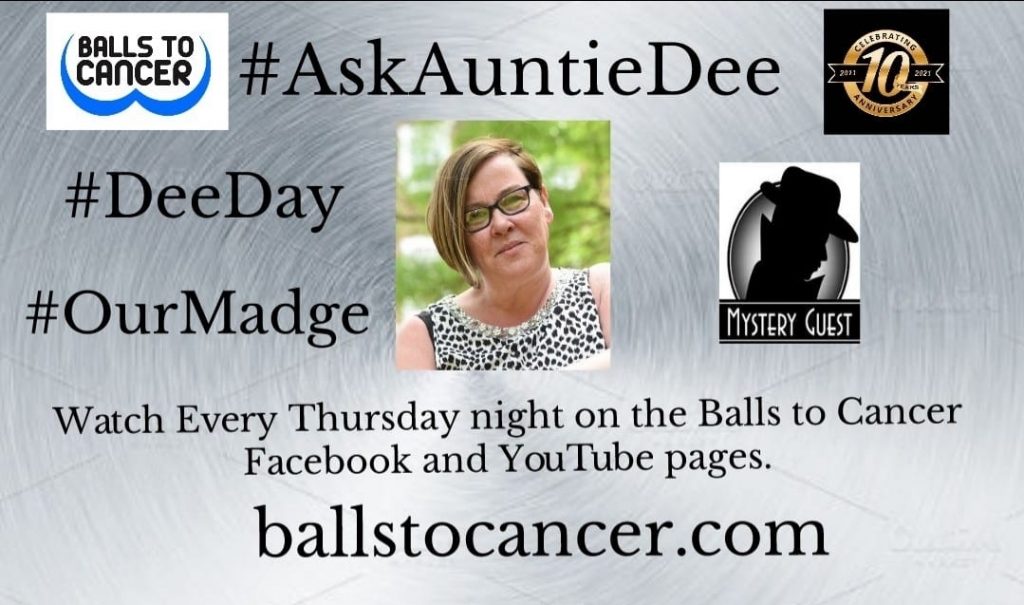
Our ambassador, Former Benefit Street and Celebrity Big Brother contestant Dee Kelly kicked off her new agony Aunt /chat show back in June 2020. The show goes out LIVE on our Facebook page here & YouTube channel here
Dee will be chatting to anyone and everyone about everything and interviewing a celebrity guest (we drop on her) every week!
So be there don’t miss out on what is always a fun night.
You got a problem yo She’ll solve it.
PREVIOUS SHOWS…
25th June First Show
2nd July (Guest Matt LeTissier)
9th July (Guest Steve Clamp)
16th July (Guest Annette Badland)
23rd July (Guest Ricky Rayment)
30th July (Guest Thomas Turgoose)
6th August (Guest Ricci Guarnaccio)
13th August ( Dee Kelly )
20th August ( Neil Razor Ruddock )
27th August (Shane Nolan)
3rd September (Charlie Lawson &Annette Badland)
10th September (Andy Whitaker)
17th September (Kellie Maloney)
24th September (Tim Healy)
1st October (Michael Starke)
8th October (Antony Costa)
15th October (Matt Hoy)
22nd October (Scott Lyons)
29th October (Deano Baily)
5th November (Cat Simmons)
12th November (Tim Hogarth)
19th November (India Willoughby)
26th November (Sean Heydon)
3rd December (Dee Kelly )
10th December (Cheryl Baker)
17th December (various guests)
7th January 21 (Ritchie Neville)
14th January (Hughie Maughan)
21st January (Rodney Marsh)
28th January (Nick & Royston)
4th February (Noel Clarke)
11th February (Cheryl Fergison)
18th February (Richard Ashton)
25th February (Mel Eves)
4th March (Trevor Michael George’s)
11th March (Jason Maza)
18th March (Ben Hanson )
25th March ( Kavana )
1st April ( Wayne Lineker)
8th April (Dominic Matteo)
15th April (Laurence Fox)
22nd April ( Apache Indian)
29th April (Andy Buchanan)
6th May (Les Dennis)
13th May (Honey G)
20th May ( Paddy Wallace)
27th May (Harry Visinoni)
3rd June (Sian Reeves)
10th June (Vicki Michelle)
17th June (Monty Panesar and Leo Goldenchild)
24th June (Tom Varndell) 1st Anniversary with surprise guests Fat Scottie and Ricci Guarnaccio
1st July BTC FC Manager (Larry Adeyanju)
8th July (Dee and Madge )
15th July ( Akeem Griffiths)
22nd July (Auntie Dee & Friends)
29th July ( Matt Jarvis )
5th August (Stephen K Amos )
12th August (Dean Windass)
19th August (Professor Karol Sikora)
26th August (Robin Windsor)
2nd September (Stuart Wolfenden)
9th September (Scott Kyle)
16th September (Sian Reeves) take 2
23rd September (Raurie “NoHun” Williams)
30th September (Dee chats to the BTC Family)
The 2.2 million people who have been self-isolating in England during the pandemic will no longer need to shield from 1 August.
From 6 July, they will be able to meet up outdoors, in a group, with up to five others and form ‘support bubbles’ with other households.
The measures can be eased because infection rates are falling, the government says.
Support packages will remain until the end of July to help people transition.
Those who are shielding and live alone in England – including single parents who are shielding – will be able to create a support bubble with one other household of any size.
This follows the ‘social bubble’ rules which were introduced earlier this month for anyone living alone and single-parent households.
People shielding will also be able to meet in groups of up to six outdoors while maintaining social distancing rules.
Still shielding: ‘The novelty has certainly worn off’
Extremely vulnerable people who are most at risk from becoming ill from coronavirus will no longer need to shield in England.
That means they can return to work, if they can’t work from home, as long as their workplace is COVID secure .
However, they should still follow social distancing guidelines when outside their homes and wash their hands regularly to reduce the risk of being infected.
The changes mean those shielding will no longer be eligible for statutory sick pay – unless they develop coronavirus symptoms, or someone they know develops symptoms, and they are told to self-isolate and cannot work from home.
Free essential food boxes will stop being delivered, but support from NHS volunteers and local councils is still possible.
They will still qualify for priority slots for online shopping and will be offered help with medicine deliveries and getting to medical appointments.
The UK government says the advice can be relaxed because the chances of encountering the virus in the community continue to fall – one in 1,700 people are estimated to have the virus now, down from 1 in 500 four weeks ago.
The government says it has worked with clinicians, GPs, charities, the voluntary sector and patient groups on the changes.
But some charities are criticising the relaxing of the advice, saying many of the people they support do not feel it is safe to stop shielding.
“We know how difficult this period has been and the impact shielding has had on many people’s mental health,” says Dr Jenny Harries, deputy chief medical officer.
“We believe it is the right time to relax some of the advice so people can start to regain a degree of normality once more in their daily lives.”
But she added the advice on shielding could change again “if there are any changes in the rates of infection that could impact on this group”.
As the country went into lockdown, around two million people were sent letters by their GPs telling them not to leave home and to avoid contact with others.
This was to protect them from the virus because they were considered to be most at risk from Covid-19.
Among the list of people who should be shielding are solid organ transplant recipients, cancer patients undergoing chemotherapy, pregnant women with heart disease and people with severe respiratory conditions such as cystic fibrosis and severe asthma.
Over half of those shielding are under the age of 70; more than 90,000 are children.
Since the start of June, people shielding in England were told they could go out once a day – to meet one person from another household while adhering to social distancing.
From the beginning of August, that shielding advice is to be completely relaxed.
The NHS will keep the shielded list, in case more advice needs to given to this group in future.
Northern Ireland has already said people will no longer need to shield from 31 July.
But officials say this pausing of the advice will only happen if the rate of community transmission remains low.
People who are shielding and living alone in Northern Ireland will also be able to form a support bubble from 6 July with one other household.
Until then, people shielding across the UK are advised to stay at home as much as possible and to practise social distancing when they go outside.
In Scotland, the advice applies to around 180,000 people and is in place until at least 31 July.
Meanwhile in Wales, almost 130,000 people are shielding and the Chief Medical Officer for Wales says the current guidance runs until at least 16 August.
Source : BBC